Key takeaways
- Suboxone (buprenorphine/naloxone) is a prescription drug that treats opioid use disorder in adults. Suboxone comes as a film that dissolves in your mouth. It’s usually taken once per day.
- Treatment has two phases: induction, to manage withdrawal, and maintenance, to sustain recovery. Typical maintenance dosages are between 4 mg buprenorphine/1 mg naloxone and 24 mg buprenorphine/6 mg naloxone once per day, which is also Suboxone’s maximum dosage.
- Abruptly stopping Suboxone can cause withdrawal, so doctors gradually reduce (taper) the dosage to end treatment. A dosage taper helps prevent withdrawal.
Suboxone is a prescription medication used to treat opioid use disorder (OUD) in adults. OUD is a medical condition that includes both physical dependence on opioids and behavioral symptoms like cravings and difficulty managing use. If you suddenly stop using opioids, withdrawal symptoms may occur.
Suboxone is a combination drug containing the active ingredients buprenorphine and naloxone. Buprenorphine is a partial opioid agonist. It produces mild opioid effects while blocking stronger opioids from attaching to receptors. Naloxone is an opioid antagonist. It blocks opioids from attaching to receptors.
This article describes the dosages of Suboxone, as well as its strengths and how to take it.
Suboxone treatment for opioid use disorder has two phases: induction, to manage withdrawal, and maintenance, to sustain recovery. Your doctor will start you on a low dosage and adjust it over time to reach the right amount for you.
The following information describes dosages that are commonly prescribed or recommended for Suboxone. But be sure to take the dosage your doctor prescribes for you. They’ll determine the best dosage to fit your needs.
Suboxone form
Suboxone comes as a film that dissolves under your tongue (sublingual) or between your cheek and gums (buccal).
Suboxone strengths
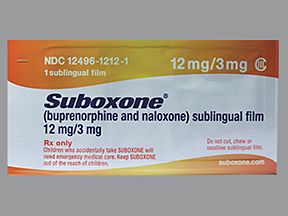
Suboxone comes in four strengths:
- 2 milligrams (mg) buprenorphine/0.5 mg naloxone
- 4 mg buprenorphine/1 mg naloxone
- 8 mg buprenorphine/2 mg naloxone
- 12 mg buprenorphine/3 mg naloxone
Treatment for opioid use disorder occurs in two phases: induction and maintenance. Your doctor will closely supervise your medical treatment to manage your withdrawal symptoms.
The second phase of treatment is called the maintenance phase. You’ll be on a stable dosage of Suboxone during the maintenance phase. You’ll continue to meet with your doctor at least once per week during the first month of treatment.
Induction dosage
Suboxone is used to manage withdrawal symptoms during the induction phase for short-acting opioids only. Short-acting opioids include heroin, codeine, oxycodone (Oxycontin, Roxicodone), and morphine (MS Contin). (For long-acting opioids, see the “Note” later.)
During the induction phase, Suboxone should be dissolved under the tongue.
On the first day, your doctor will start treatment with one of the following strengths of Suboxone: 2 mg buprenorphine/0.5 mg naloxone or 4 mg buprenorphine/1 mg naloxone.
Your care team will monitor you for several hours. Your doctor may give you additional doses to treat withdrawal symptoms. The maximum dosage of Suboxone for the first day is 8 mg buprenorphine/2 mg naloxone.
On the second day, your doctor may give you the total dose of Suboxone you received on the first day. But if you’ve had significant withdrawal symptoms, your doctor may increase this dose by 2 mg buprenorphine/0.5 mg naloxone or 4 mg buprenorphine/1 mg naloxone.
Again, your doctor may give you additional doses if needed.
This process may continue for additional days until your withdrawal symptoms are effectively managed and your care team determines the correct dose of Suboxone for you. You’ll then take this dose once per day as your maintenance dosage. The maximum dosage of Suboxone for the second day is 16 mg buprenorphine/4 mg naloxone.
Note: For dependence on long-acting opioids such as methadone, doctors prescribe a 2-day induction of buprenorphine alone before prescribing Suboxone as a maintenance therapy.
Maintenance dosage
Once you start your maintenance dosage for opioid use disorder, you can dissolve Suboxone under your tongue or between your cheek and gums. (The “How to take Suboxone” section explains this.)
Typical maintenance dosages of Suboxone are between 4 mg buprenorphine/1 mg naloxone and 24 mg buprenorphine/6 mg naloxone once per day. However, your dosage will depend on your body’s response to treatment. The highest daily dose of Suboxone for maintenance therapy is 24 mg buprenorphine/6 mg naloxone.
Dosage adjustments
If you’re pregnant and taking Suboxone, you should meet with your doctor regularly. During pregnancy, your doctor may need to adjust your Suboxone dosage. If you experience any withdrawal symptoms during pregnancy, tell your doctor.
Here are answers to some commonly asked questions about Suboxone’s dosage.
What do I do if my Suboxone dose is too low?
If your Suboxone dose is too low, tell your doctor right away. Signs and symptoms that your dose may be too low include:
Symptoms are similar but tend to be milder than typical opioid withdrawal symptoms.
If you think your Suboxone dosage is too low, do not increase your dose on your own. Talk with your doctor as soon as you can.
Can Suboxone be taken for pain? If so, what’s the dosage?
Suboxone may be used off-label for treating chronic (long-term) pain in people with opioid use disorder. With off-label use, doctors prescribe a drug for a purpose other than what it’s approved for.
Suboxone isn’t used as pain medication in people who don’t have opioid use disorder. It hasn’t been effective as pain management in this group of people.
One of the ingredients in Suboxone, called buprenorphine, can be used by itself to treat very strong pain that isn’t helped by other pain medications. But there have been reports of people dying when it was given to those who don’t regularly take opioids. This is because their bodies weren’t used to the strong effects of the drug.
Drug manufacturers don’t provide dosage recommendations for off-label uses. But if you’d like to learn more about treating your pain with Suboxone, talk with your doctor.
What if I miss a dose of Suboxone?
If you miss a dose of Suboxone, take it as soon as you remember. But if it’s almost time for your next dose, skip your missed dose and take your next dose at its regularly scheduled time. You should not take two doses of Suboxone at once. If you’re not sure if you should take a missed dose or skip it, talk with your doctor or pharmacist.
If you need help remembering to take your dose of Suboxone on time, try using a medication reminder. This can include setting an alarm or downloading a reminder app on your phone.
Optum Now is operated by RVO Health. By clicking on this link, we may receive a commission. Learn more.
Once you’re on your maintenance dosage, you’ll take Suboxone once per day.
Suboxone comes as a film that dissolves under your tongue or between your cheek and gums. It should be taken whole. Do not cut, chew, or swallow the film. Do not eat or drink anything until the film has completely dissolved. Do not move the film after it’s been placed in your mouth.
For placement under the tongue: Place one film under your tongue. If you need more than one film to complete your dose, place them both under the tongue — one on the right side and one on the left side. Try to avoid having the films overlap. Keep the film under your tongue until it has completely dissolved. If you need a third film, follow the same steps but only after the first two films have dissolved.
For placement between the cheek and gums: Place one film on the inside of the cheek, between the cheek and gums. If you need more than one film to complete your dose, place it on the inside of the opposite cheek. Keep the film in place until it has completely dissolved. If you need a third film, follow the same steps but only after the first two films have dissolved.
After the film has completely dissolved, take a sip of water and gently swish the water around your teeth and gums. Swallow the water.
Wait at least 1 hour before brushing your teeth.
How long do you take Suboxone?
Suboxone is usually a long-term treatment. If you and your doctor determine that Suboxone is safe and effective for your condition, you’ll likely take it long term.
Yes, Suboxone has the potential for misuse. With misuse, a person takes a drug in a way other than how it’s prescribed.
Suboxone contains the active ingredient buprenorphine. The federal government has classified buprenorphine and all drugs that contain buprenorphine as Schedule III drugs. This means Suboxone has moderate potential for misuse.
Your doctor will take certain precautions to minimize the risk of misuse. Initial precautions may include:
- giving you the medication under supervision
- prescribing a limited supply of Suboxone at once
- scheduling frequent follow-up appointments
- requesting urine drug screening
As you progress in your treatment, these precautions may no longer be necessary.
Do not take more Suboxone than your doctor prescribes, as this can lead to harmful effects.
Symptoms of an overdose
Symptoms caused by an opioid overdose can include:
- small pupils
- stupor (unresponsiveness to typical conversation)
- slow and ineffective breathing
- slow heart rate or weak pulse
A severe overdose can lead to low blood pressure, respiratory arrest (no breathing), coma, and even death.
What to do in case you take too much Suboxone
Call your doctor right away if you think you’ve taken too much Suboxone. You can also call 800-222-1222 to reach America’s Poison Centers or use its online resource.
Due to the risk of opioid overdose in people being treated for opioid use disorder, your doctor may have given you a prescription for naloxone (Narcan). Your companions should be educated on the signs of an opioid overdose and how to give naloxone.
In the event of an opioid overdose, a companion should immediately administer naloxone if it’s available. They should then call 911 (or the local emergency number) or bring you to the nearest emergency room.
If you abruptly stop taking Suboxone, you may experience moderate withdrawal symptoms. This is because buprenorphine, one of the active ingredients in Suboxone, has the potential for dependence. With dependence, your body needs the drug to function as usual.
Withdrawal symptoms tend to be their worst after 3 or 4 days and could last up to 2 weeks. Symptoms include:
- nausea
- headache
- diarrhea
- flu-like symptoms
- sweating
- muscle aches
- anxiety
- restlessness
- yawning
- running nose
- drug cravings
When you and your doctor decide to stop Suboxone, it can be done safely with a drug taper. With a drug taper, your dose is slowly decreased over several weeks. This helps decrease withdrawal symptoms and increases your chance of successfully stopping Suboxone.
The sections mentioned earlier describe the usual dosages provided by the drug’s manufacturer. If your doctor recommends Suboxone for you, they’ll prescribe the dosage that’s right for you.
Remember, you should not change your dosage of Suboxone without your doctor’s recommendation. Only take Suboxone exactly as prescribed. Talk with your doctor if you have questions or concerns about your current dosage.
Here are some examples of questions you may want to ask your doctor:
- How do I know if my Suboxone dosage is right for me?
- How long will I receive Suboxone in my doctor’s office?
- Does it make a difference if I place the film under my tongue or inside my cheek?
- Does my risk of dependence increase if I’m prescribed a higher dosage of Suboxone?
To get information on different conditions and tips for improving your health, subscribe to any of Healthline’s newsletters. You may also want to check out the online communities at Bezzy. It’s a place where people with certain conditions can find support and connect with others.
Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.